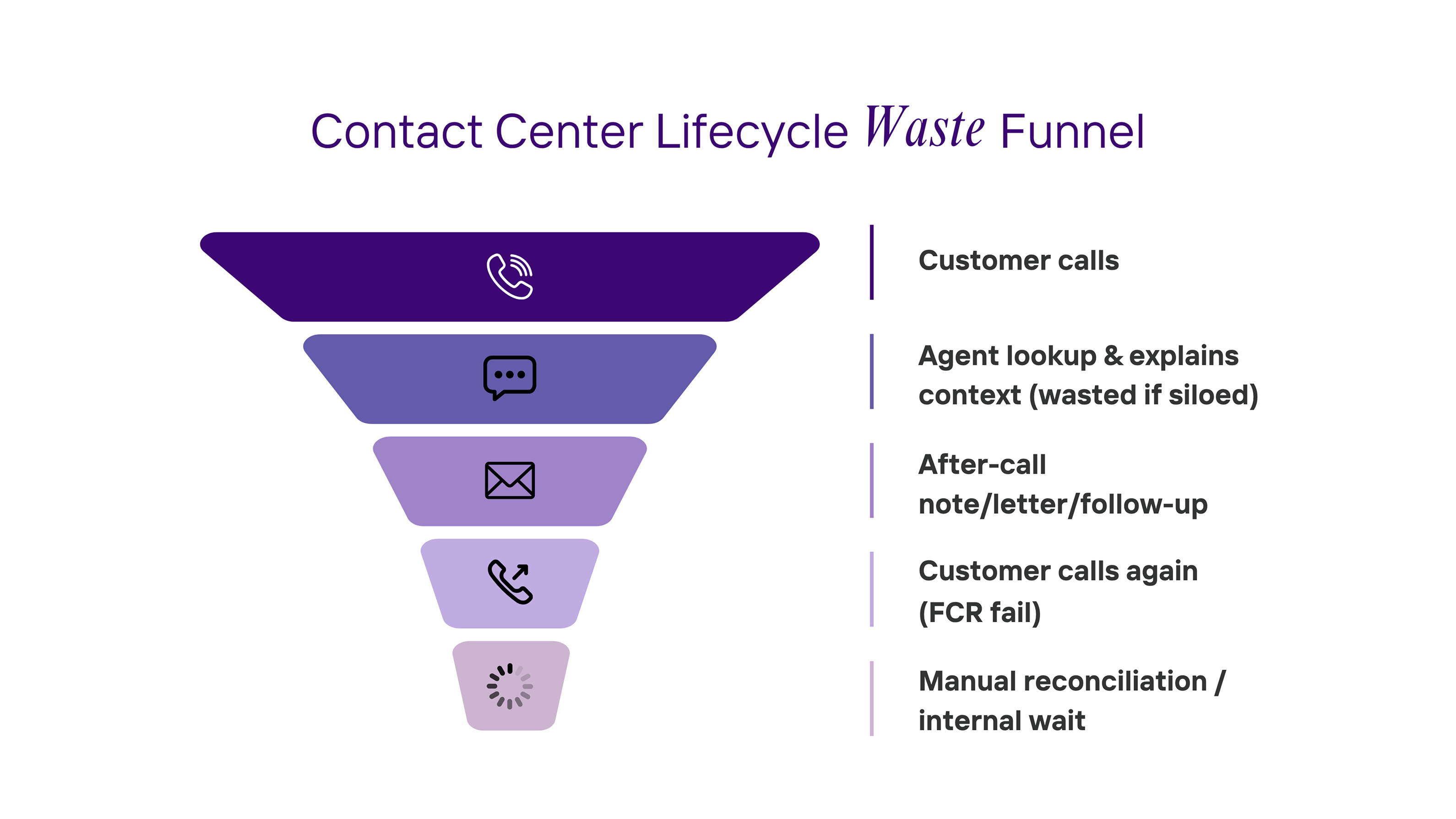
Insurance operations leak value long before a claim is adjusted. The biggest drains live in non-claims work: contact centers (policy/billing/status), policy servicing, endorsements, agent/broker support, directory compliance, and third-party verification calls. The pattern is consistent: repeat contacts, after-call busywork, manual chase work, and waiting for internal responses.
A few grounding facts:
What that implies (illustrative math): If a CSR handles ~75 customers/day at ~6.1 min each, and 31% of those are repeat contacts (because FCR=69%), that’s ~2.36 hours/day burned on avoidable repeats — ~615 hours/year per agent. At typical insurance CSR wages, that’s ~$13.7k–$14.2k per seat per year just from repeat contacts — before any ACW reduction. (eCommons)
Add a realistic 50% cut to ACW (e.g., AI-filled notes/templates), and you can free another ~122–244 hours/agent/year (≈ $2.7k–$5.6k). (VoiceSpin)
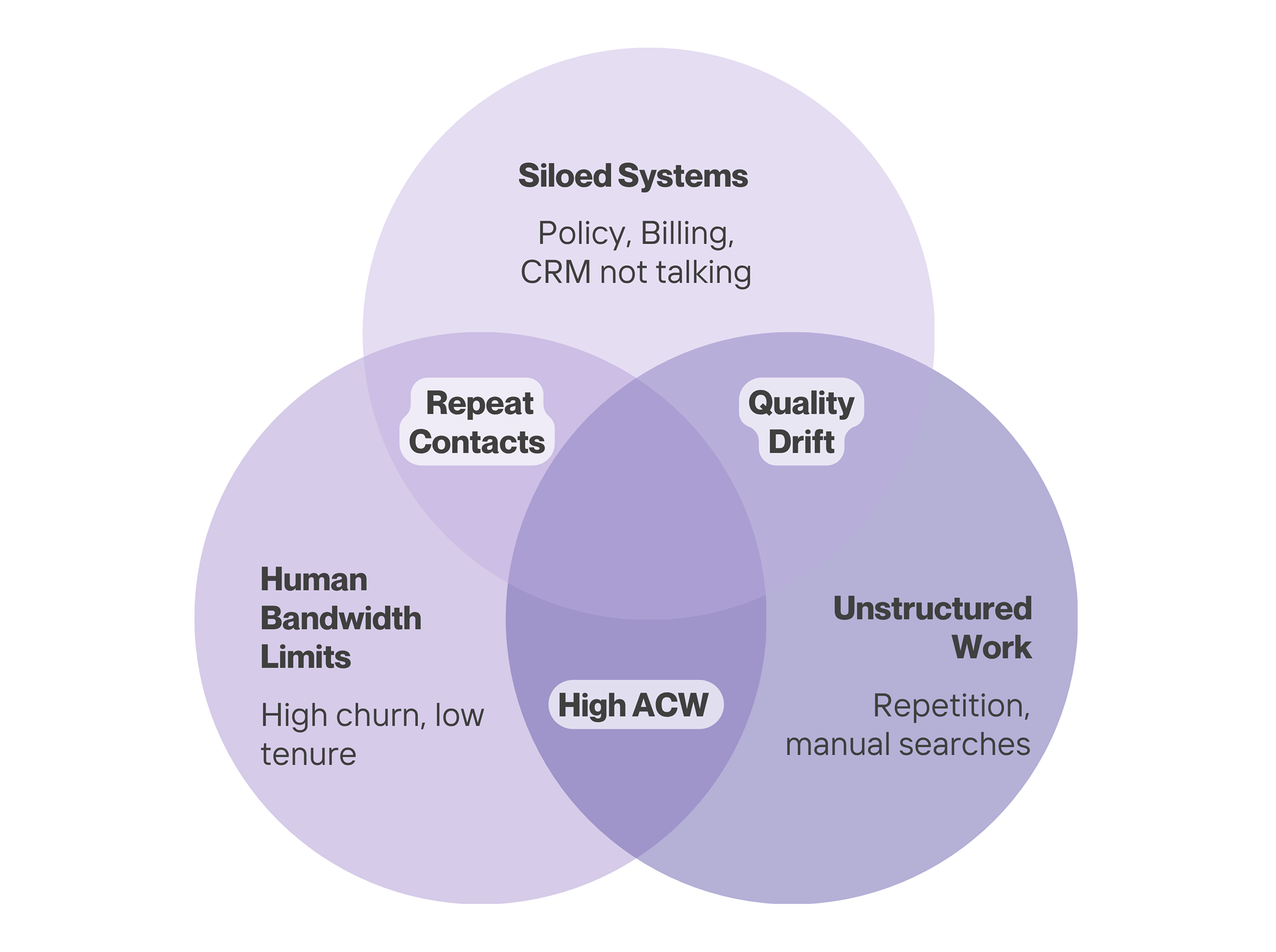
Wasted time drivers
Why this matters economically
Extra pressure points
Wasted time drivers
Wasted time drivers
Wasted time drivers
Inputs (from research):
Illustrative outputs (per seat/year):
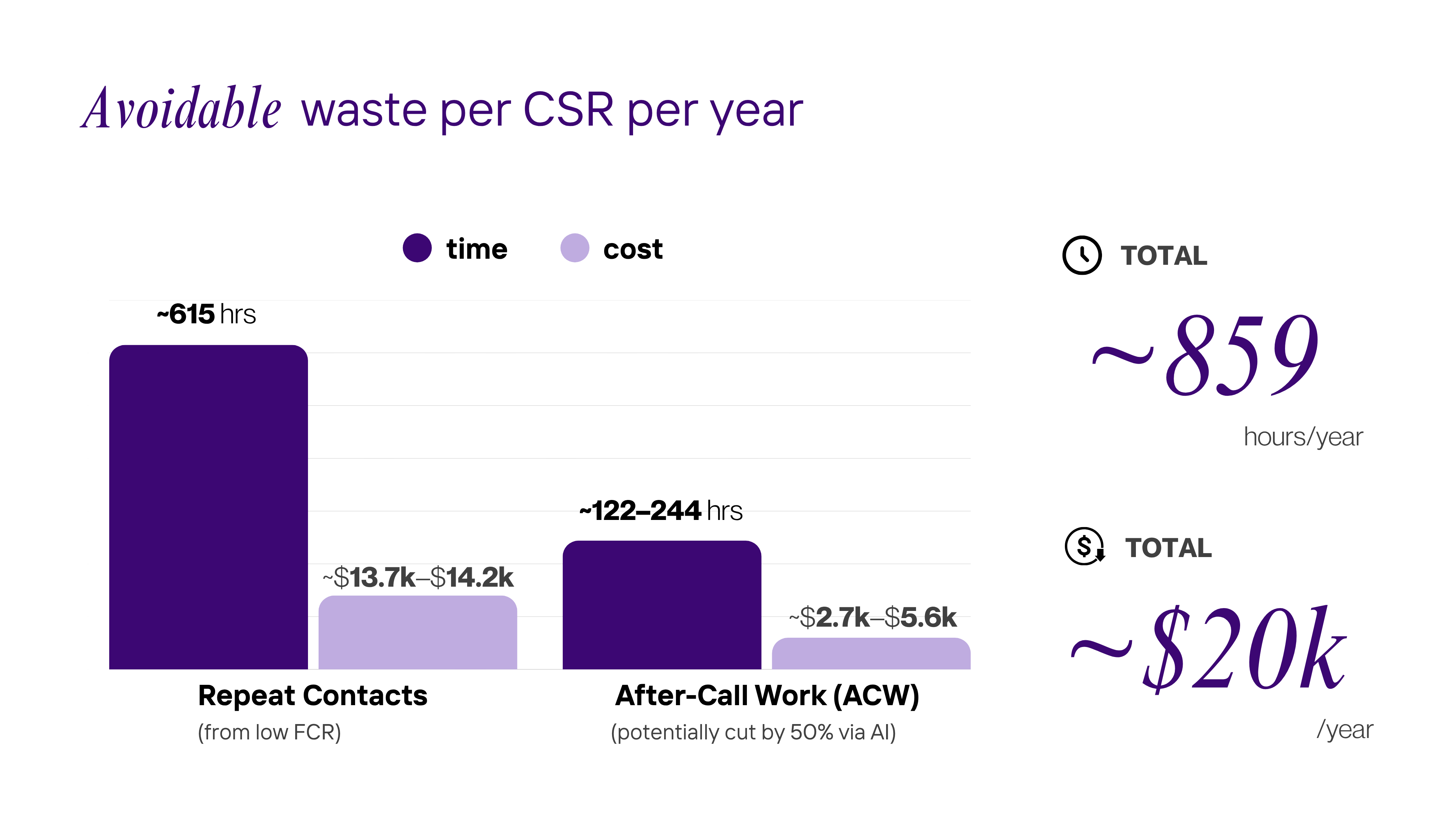
Takeaway: The “non-claims tax” in policy/billing/status work is five figures per agent per year in avoidable labor — even before considering attrition backfill, QA leakage, or dissatisfied members calling again.
AIBPO’s promise: We own the grunt work; you keep the decisions.
Why it pays back quickly (using the research above):
We’ll plug your FCR, AHT, ACW, volumes, and wage data into the same transparent model to project savings by month/line of business — then stand up a 6-week lighthouse (top 4–5 inquiry types) to prove it in production.
.svg)
.svg)
.svg)



