“Three-point contact” (reaching the injured worker/claimant, employer/other party, and treating provider/third party within the first day or two) is a bedrock claims best practice. Many carriers/TPAs still miss it consistently—not for lack of will, but because adjusters burn hours dialing gatekeepers, leaving voicemails, chasing fax/portal confirmations, and re-keying notes. Research and regulatory guidance make two things clear:
Below, I unpack what three-point contact is, why it’s hard in practice, the business impact of missed contact, and how an AI-plus-human model (AIBPO) removes the waste while improving auditability.
In workers’ comp (and many liability lines), three-point contact is early, live contact with:
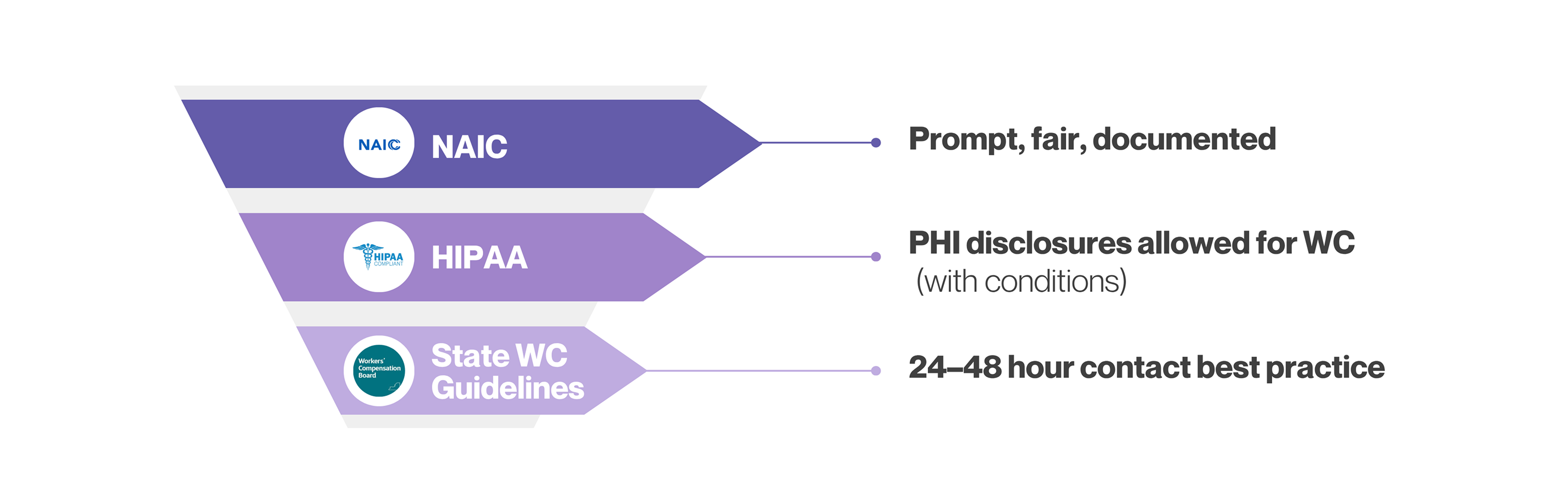
Authoritative manuals and industry guidelines commonly set 24 hours (sometimes 48 hours) from assignment as the target. The Massachusetts WC Best Practices Manual, for example, calls for a three-point investigative review within 48 hours and 24-hour internal review, while other published best-practice checklists specify voice contact with all three within 24 hours. (eservices.hrd.state.ma.us)
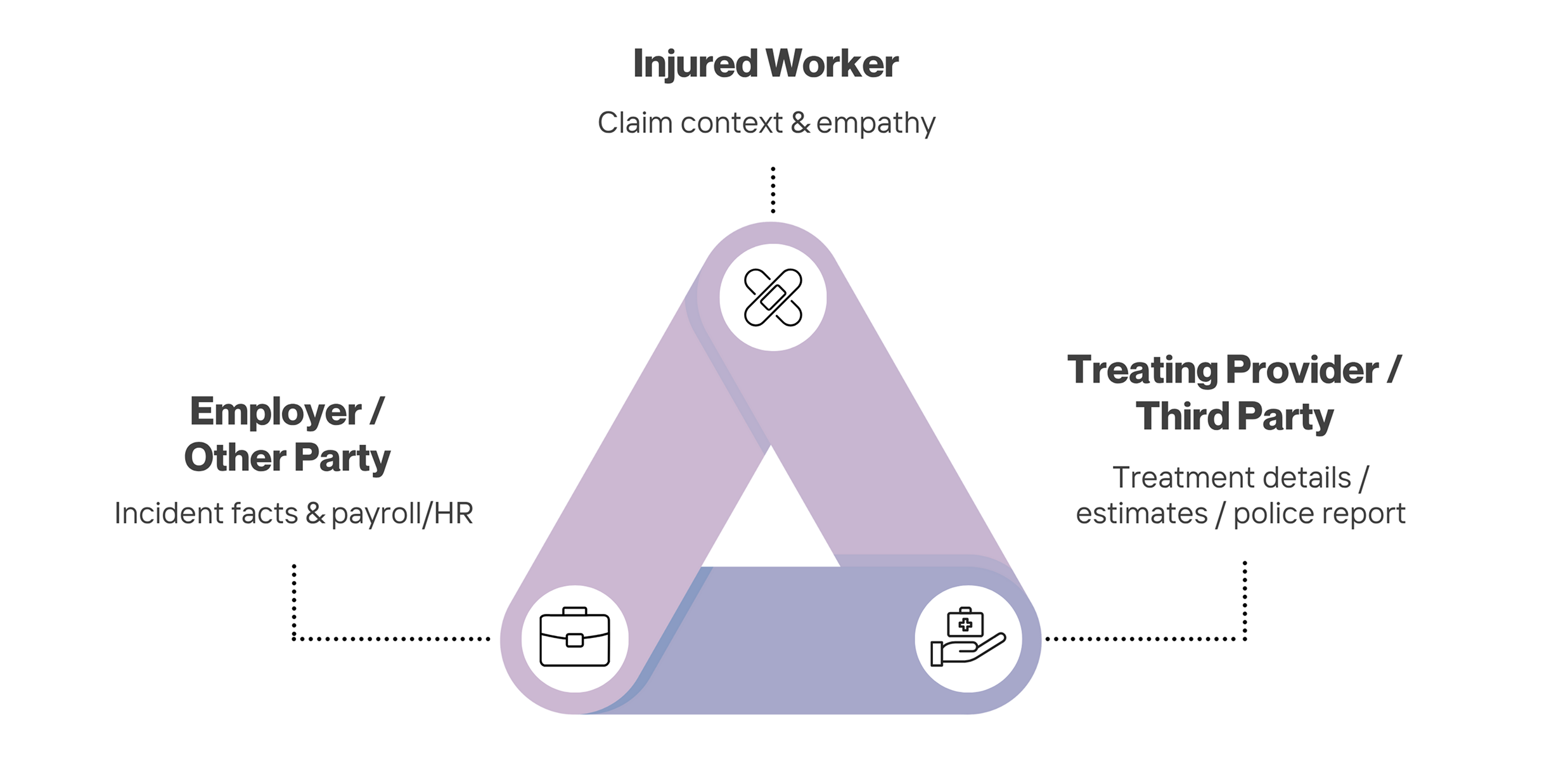
Early, empathetic contact sets expectations, reduces misinformation, and accelerates compensability and treatment decisions. Industry research links delayed engagement with higher rates of attorney involvement and longer, costlier claims. WCRI’s recent study on lawyer involvement quantifies how attorney representation materially increases indemnity and duration; early adjuster contact is one of the practical levers to avoid that path. (WCRI)
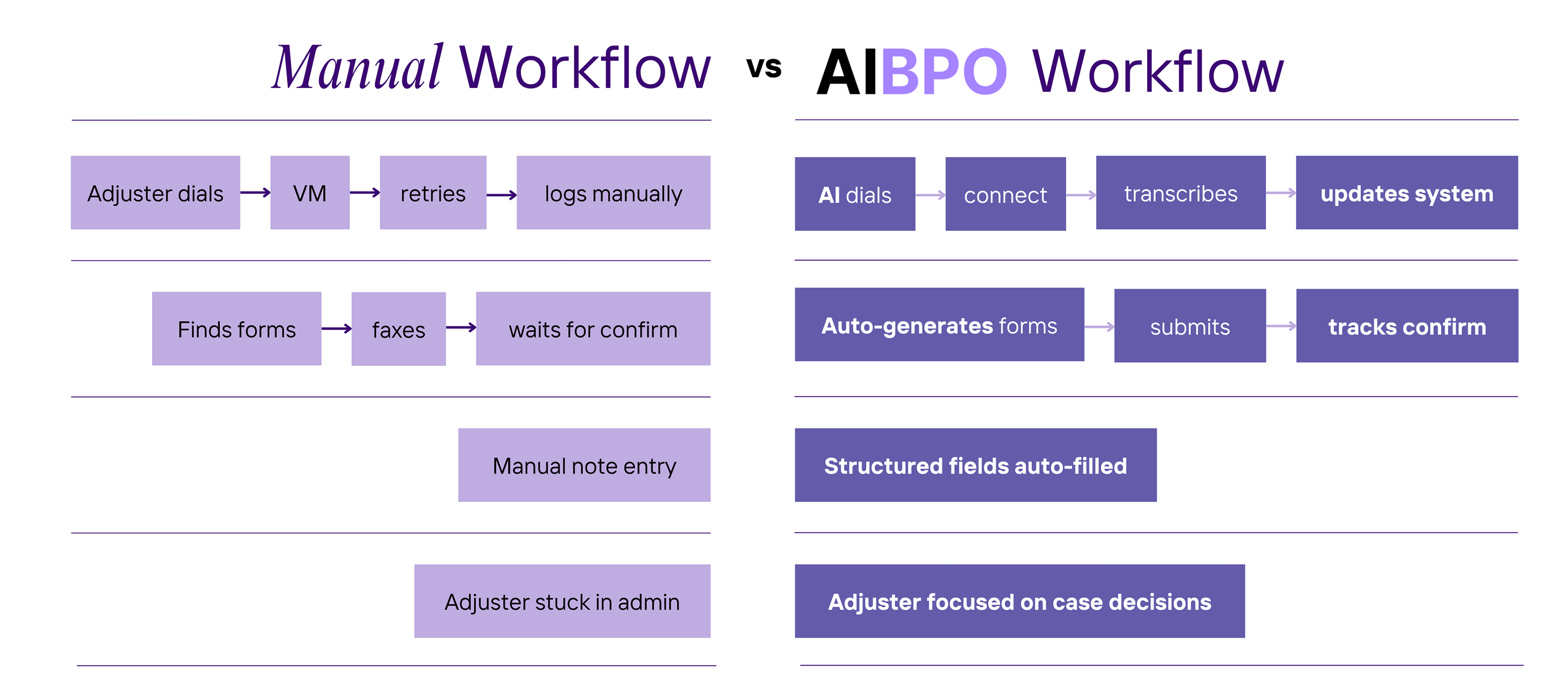
Talk to any experienced adjuster and you’ll hear the same culprits:
None of this uses the adjuster’s highest-value skills (liability analysis, negotiation, human empathy in difficult moments). McKinsey’s claims research underscores the broader point: a big chunk of claims work is administrative and ripe for automation and redeployment of human time. (McKinsey & Company)
Even outside CAT events, U.S. carriers/TPAs face millions of events that trigger verification calls annually:
In both segments, each claim can require 3+ outbound contacts—and often more (shops, contractors, municipal records, other carriers). That’s why “just a few extra minutes” per call becomes a major leakage source across a book of business.
Regulators don’t prescribe “24 hours” universally, but they do require prompt investigations and fair claim handling. The NAIC’s Unfair Claims Settlement Practices Act and related Model Regulations codify minimum standards for prompt, equitable settlements and investigations—so carriers need both speed and audit-ready documentation of their outreach. (NAIC)
For medical information in workers’ comp, HIPAA is not a barrier to early coordination: HHS guidance explicitly allows disclosures for workers’ compensation purposes without the individual’s authorization when permitted or required by WC law—again, with documented, minimum-necessary handling. (HHS.gov)
A practical way to size the “waste” is to look at the portion of claims labor tied to these verification and documentation tasks.
Total serviceable labor TAM for “verification work” ≈ $6.9–$7.0B per year (U.S.). Using even stricter filters (only some lines, lower time shares) still lands in the multi-billion range.

A Verification Packet for each claim that your adjusters can rely on without re-calling third parties:
Three-point contact isn’t glamorous, but it’s where money and customer experience are won or lost. The research is unambiguous: do it early and do it right. Let your adjusters focus on the calls only they should make—and let AIBPO industrialize everything else.
Ready to see it? We’ll pilot on a subset of claims and report time-to-contact, cycle time, first-pass completeness, and exception rate after 30 days—along with the full audit log your compliance team will love.
.svg)
.svg)
.svg)



